Abstract
We have earlier shown that early use of prophylactic G-CSF mobilized DLI resulted in improved disease-free survival following post-transplantation cyclophosphamide (PTCy) based haploidentical HSCT in patients with relapsed/refractory myeloid malignancies. CD56 enriched donor cell infusion following PTCy for similar cohort resulted in rapid proliferation of mature NK cells with attenuation of GVHD. However, the relapse rate was higher than that with early DLI (50% vs 21.4%). CTLA4Ig has been shown to be effective in attenuating T cell activation and induce transplantation tolerance in preclinical models. NK cells on the other hand are resistant to CTLA4Ig and in fact might demonstrate better anti-tumour effect in presence of CTLA4Ig as CD86 is a putative activation receptor. To explore this phenomenon, we employed sequential CTLA4Ig primed DLI following PTCy based haploidentical HSCT.
The study group (CTLA4Ig-DLI) had 24 patients (4-65 years; myeloid malignancies-10, Lymphoid malignancies-14) received Abatacept (CTLA4Ig) at 10 mg/kg on day -1 followed by PBSC and sequentially on days +6, +20 and +35 followed 12 hours later by DLI of 5 x 106 CD3 cells/kg containing 0.03-1 x106/kg CD56+ cells. PTCy was administered on days +3 and +4 with cyclosporine from day +5 to day +60 and subsequent rapid tapering. The outcome and immune reconstitution of the CTLA4Ig-DLI group was compared with the cohort of patients who received DLI without abatacept (n=21; DLI group)
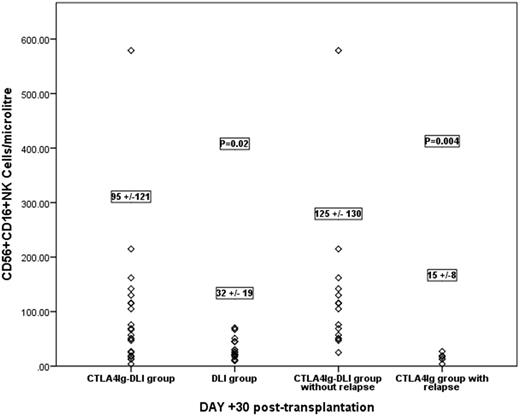
All patients engrafted at a median of 15 days (11-20 days). The incidence of acute GVHD was 9.7% compared to 31% in the DLI group (p=0.08) and that of chronic GVHD was 28% vs 41.2% (p=0.4). Three patients required treatment for CMV infection with no non-relapse mortality (0% vs 19.9% in DLI group; p=0.03). The relapse incidence was 25.4% vs 21.4% in the DLI group (p=0.7) with an overall survival of 82% vs 70.5% at 18 months (p=0.4). In the CTLA4Ig-DLI group only 1/10 patients with myeloid malignancies relapsed compared to 5/14 in the lymphoid group. Absolute CD56+CD3- and CD56+CD16+ NK cells were significantly higher in the CTLA4Ig-DLI group at day +30 (175±162 vs 73±34; p=0.008 and 95±121 vs 32±19.1; p=0.02 )and +60 (134±107 vs 98±55; p=0.1 and 84 ±87 vs 30±10; p=0.01). The CD56+16+ NK cell population in the CTLA4Ig-DLI group had a higher expression of KIR receptors at day +30. Within the CTLA4Ig-DLI group, patients not experiencing relapse had a significantly higher CD56+16+ NK cell populations at day +30 (125±130 cells/microl vs 15 ± 8±; p=0.004) and day +60 (104±93 cells/microl vs 25± 16; p=0.006).
CTLA4Ig primed DLI resulted in greater proliferation of NK cells with mature phenotype than the DLI group with comparatively lower incidences of acute GVHD and NRM and improved relapse-free survival, particularly in those with myeloid malignancies. Higher proliferation of mature NK cells at 30 and 60 days post-transplant was associated with a lower risk of relapse following CTLA4Ig primed DLI. Thus, this novel approach enabled early institution of adoptive immunotherapy to mitigate the risk of relapse in advanced leukemia without increase in GVHD or NRM.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal